
Tackle Perimenopause Weight Gain in the Belly with Practical Tips
Share
If you've noticed a frustrating shift in how your body stores weight, you're not imagining things. That stubborn perimenopause weight gain belly is a real and common experience, driven by a complex hormonal transition. It's not just about diet or exercise, and the strategies that worked in your 30s often just don't cut it anymore. This is a new chapter, and it requires a new approach.
Why Does Weight Settle In Your Belly During Perimenopause?
It can feel incredibly disheartening when you’re doing everything "right"—eating well, staying active—only to see the number on the scale creep up and your waistline expand. This change isn't a reflection of your effort. It’s a biological response to the hormonal shifts defining this new chapter of your life.

As you enter perimenopause, your estrogen levels begin to decline erratically. This single change sets off a cascade of events that literally reshapes your body. Think of estrogen as a traffic controller for fat storage; when it was abundant, it directed fat to your hips and thighs. Now, with less of it on duty, your body defaults to a different storage pattern, sending fat directly to your abdomen.
The Hormonal Blueprint for Belly Fat
This isn't just about the soft, pinchable fat under the skin. The hormonal changes also encourage the storage of visceral fat, a deeper, more metabolically active type of fat that wraps around your internal organs. This is why managing perimenopause weight gain is crucial not just for how you feel in your clothes, but for your long-term health and longevity. Our guide on what visceral fat is and why it matters explains this in greater detail.
To put it simply, your body is operating under a new set of rules. Understanding them is the first step toward regaining a sense of control.
It's a Numbers Game, Too
Statistics from credible research show just how common this is. Approximately 70% of women experience weight gain during perimenopause, with a notable increase in abdominal fat. As estrogen declines, body fat can increase by about 1.7% each year, while metabolism-supporting muscle mass decreases. It's a double whammy that makes weight management feel like an uphill battle.
Let's break down the key biological drivers at play.
Key Drivers of Perimenopause Belly Fat
| Hormonal and Metabolic Factor | Impact on Your Body |
|---|---|
| Declining Estrogen | Changes fat distribution, shifting it from the hips and thighs directly to the abdomen. |
| Increased Cortisol | Stress levels often rise, and this "stress hormone" is directly linked to storing deep visceral fat in the belly. |
| Insulin Resistance | Your body becomes less efficient at managing blood sugar, which can trigger more fat storage, especially around the middle. |
| Slowing Metabolism | Age-related muscle loss (sarcopenia) accelerates, causing your body's calorie-burning engine to slow down significantly. |
| Poor Sleep | Fluctuating hormones disrupt sleep, which in turn messes with appetite-regulating hormones like ghrelin and leptin, leading to cravings and overeating. |
These factors work together, creating a perfect storm for abdominal weight gain.
This biological reality means it’s time for a new playbook. For a deeper dive into women's health concerns during these transitions, you can explore insights from a holistic health coach on menopause and weight loss.
In the sections ahead, we'll explore the science-backed solutions that actually work with your body's new chemistry, not against it.
How Hormones Reshape Your Metabolism
During perimenopause, it can feel like your body's internal thermostat has gone haywire. The metabolic rules you’ve lived by for decades don't seem to apply anymore, and the main reason for this shift is a major shake-up in your hormonal orchestra. The first step to working with your body, not against it, is understanding who the key players are.

Think of your metabolism like a bustling factory. For most of your adult life, estrogen was the highly efficient factory manager, expertly directing how energy (calories) was used and where any extra resources (fat) were stored—usually around the hips and thighs. As estrogen levels begin to drop, it’s as if the manager has left the building. The factory defaults to a new, less efficient system: storing fat centrally, right around your abdomen.
Estrogen's Exit and Fat Storage
The decline in estrogen does more than just reroute fat storage; it also slows down your overall metabolic rate. This means your body naturally burns fewer calories at rest than it once did. Even if your diet and exercise habits haven't changed one bit, this hormonal shift alone can lead to that frustrating perimenopause weight gain belly.
This metabolic slowdown is made worse by another crucial change: your body becomes less sensitive to insulin. Insulin is the hormone that acts like a key, unlocking your cells to let sugar in for energy. When your cells become resistant to insulin's signal, your pancreas has to pump out more of it to get the job done. This creates a vicious cycle that encourages even more fat storage around your midsection.
This growing insulin resistance is often why you might suddenly get intense cravings for sugar and carbs. Your body is struggling to get fuel into its cells, so it sends powerful signals to your brain demanding a quick energy fix.
The Supporting Cast of Hormones
While estrogen grabs the spotlight, other hormones play powerful supporting roles in this metabolic drama. Each one has a unique effect on how you feel and how your body handles weight during this time.
- Progesterone: Known as the "calming" hormone, progesterone levels also fall during perimenopause. Low progesterone can lead to water retention and bloating, making your belly feel fuller and more uncomfortable.
- Testosterone: Women produce testosterone, too, and it’s vital for maintaining muscle mass. As your testosterone-to-estrogen ratio changes, you can lose muscle more quickly. Since muscle burns more calories than fat, losing it further slows your metabolism.
- Cortisol: Often called the "stress hormone," cortisol can spike during midlife due to poor sleep, hot flashes, and the general pressures of life. High cortisol is like a magnet for abdominal fat, specifically telling your body to store energy as deep, dangerous visceral fat.
This tangled web of hormonal changes creates a perfect storm for weight gain around the middle. If you think hormonal imbalances are a factor, checking your thyroid health is a smart move, as it also plays a huge role in metabolism; you can explore private thyroid testing to get a clearer picture.
Your metabolism isn't broken—it’s just adapting to a completely new set of instructions. Understanding these powerful forces is the first step toward finding solutions that truly work.
The Lifestyle Triggers That Worsen Belly Fat
While hormones are busy rewriting the rules in the background, our daily habits can either calm the storm or make it much worse. Think of your hormones as the underlying climate change of this life stage; your lifestyle choices are the day-to-day weather. By understanding how sleep, stress, and nutrition interact with your new biology, you can start making real, meaningful changes.
This isn't just you, by the way. This is a globally recognized part of the perimenopausal transition. Credible studies show that about half of women gain at least 10 pounds during this time. The real issue isn't just the number on the scale, but where that weight settles—right around the middle—which is linked to a higher risk of cardiovascular issues down the road. You can dig deeper into these trends by exploring the World Obesity Federation's findings.
Let's break down the three biggest lifestyle triggers and, more importantly, what you can actually do about them.
The Sleep and Cravings Connection
Perimenopause is notorious for wrecking a good night's sleep. Between night sweats, anxiety, and general hormonal chaos, getting a solid eight hours can feel like a distant memory. But a restless night does more than just leave you groggy; it directly sabotages your efforts to eat well the next day.
Poor sleep throws two key appetite hormones, ghrelin and leptin, completely out of whack. Ghrelin, the hormone that screams "I'm hungry," skyrockets. At the same time, leptin, the hormone that says "I'm full," takes a nosedive. This hormonal double-whammy unleashes intense cravings for high-sugar, high-fat foods.
To get your appetite back under control, focus on these simple sleep hygiene tips:
- Create a Cool, Dark Sanctuary: Keep your bedroom cool to help dial down night sweats. Blackout curtains are your best friend here.
- Establish a Wind-Down Routine: An hour before bed, power down. Put away screens and do something calming, like reading a book, gentle stretching, or taking a warm bath.
- Be Consistent: Try to go to bed and wake up around the same time every day—even on weekends. It helps regulate your body’s internal clock.
How Chronic Stress Fuels Belly Fat
Midlife can feel like a pressure cooker. We're often juggling aging parents, career demands, and the personal journey of this transition. During perimenopause, your body's natural resilience to stress is lower, which can lead to chronically elevated levels of cortisol.
Cortisol is our "fight-or-flight" hormone, designed for short bursts of stress. But when it stays high day after day, it sends a constant signal to your body: "Store energy for an emergency!" And its favorite place to stash that energy? Right in your abdomen, as deep visceral fat.
This stress also feeds emotional eating, creating a vicious cycle. Finding healthy ways to manage your stress isn't a luxury; it's a necessity for healthy living. If this is a major hurdle for you, our guide on how to stop stress eating offers some really practical advice.
The Carb and Sugar Sensitivity Shift
Remember the days when a bowl of pasta or a slice of cake didn't seem to make a dent? Things have changed. During perimenopause, your body's relationship with carbohydrates and sugar shifts dramatically as insulin resistance starts to creep in.
This means your cells become less responsive to insulin, the hormone that ushers sugar out of your bloodstream. In response, your pancreas works overtime, pumping out more insulin. The problem is, high insulin levels are a powerful fat-storage signal. The same meal that was fine a decade ago can now have a much bigger impact on your waistline.
You don't have to banish carbs entirely, but you do need to be smarter about them.
- Prioritize Fiber-Rich Carbs: Swap out white bread and sugary cereals for whole grains, beans, and vegetables. Their fiber content helps blunt the blood sugar spike.
- Pair Carbs with Protein and Fat: A great rule of thumb is to never eat a "naked" carb. Adding a source of protein or healthy fat slows down digestion and prevents that rapid insulin surge. Think an apple with a handful of almonds, not just an apple by itself.
A New Playbook for Nutrition and Fitness
It’s time to stop fighting your body and start working with it. The diet and exercise habits from your 20s and 30s were designed for a different hormonal reality. To get a handle on that stubborn perimenopausal belly fat, you need a new playbook built around strategic nourishment and smarter movement for healthy living.
Forget about punishing, restrictive diets. Your body is already dealing with enough stress. The new goal is to eat in a way that stabilizes your blood sugar, holds onto precious muscle, and keeps you feeling full and satisfied.
Prioritize Protein to Protect Your Metabolism
Think of protein as the foundation of your metabolic engine. As we enter perimenopause, our bodies become more prone to muscle loss (sarcopenia). Because muscle is our most metabolically active tissue, losing it means we burn fewer calories at rest, making weight gain feel inevitable.
Making protein the star of every meal is your single best defense. It helps you maintain that calorie-burning muscle. On top of that, protein is incredibly satiating, which is a game-changer when you're battling hormone-driven cravings.
A great target to start with is 25-30 grams of protein at each meal. This one simple shift can make a world of difference in managing your appetite and keeping your metabolism fired up. For those looking to support their health at a cellular level, some explore options like NAD+ supplements to support their energy and longevity goals.
Make Fiber Your Best Friend
Right alongside protein, fiber is another nutritional hero during this transition. It slows down digestion, which is crucial for preventing the sharp blood sugar spikes that tell your body to store fat. A diet rich in fiber also feeds the healthy bacteria in your gut, which plays a huge role in weight management.
Here are a few simple swaps to get more fiber in your day:
- Breakfast: Instead of a plain bagel, try a bowl of oatmeal topped with berries and nuts.
- Lunch: Toss a cup of lentils or chickpeas into your salad for a satisfying boost.
- Snack: Ditch the pretzels and grab an apple with almond butter.
Rethink Your Fitness Routine
When it comes to exercise, more isn't always better—smarter is. Endless hours of cardio can actually backfire by jacking up your cortisol levels, and that stress hormone loves to store fat right around the middle. The most effective approach is a smart combination of strength training and short, intense bursts of cardio.
Strength Training is Non-Negotiable
Lifting weights—or even just using your own body weight—is the most powerful tool you have to fight age-related muscle loss. Building lean muscle is like giving your metabolism a raise. The more you have, the more calories you burn 24/7. Start with foundational moves like squats, lunges, and push-ups.
Add Short Bursts of Intensity
High-Intensity Interval Training (HIIT) is all about short periods of all-out effort followed by brief recovery. A 20-minute HIIT session can be more effective for fat loss and improving insulin sensitivity than a 45-minute jog. These quick bursts teach your body to use sugar for energy more efficiently, so less of it gets stored as fat.
A Simple Weekly Plan to Get Started
Feeling overwhelmed? Don't be. Here’s a simple, doable plan to put these actionable tips into practice this week.
| Day | Movement Focus (30-45 minutes) | Nutrition Tip |
|---|---|---|
| Monday | Full-Body Strength Training | Make sure lunch includes a solid protein source like grilled chicken or tofu. |
| Tuesday | Brisk Walk or Light Cardio | Add a tablespoon of chia seeds to your morning smoothie or yogurt for a fiber kick. |
| Wednesday | Full-Body Strength Training | Have a protein-rich snack like Greek yogurt in the afternoon to curb pre-dinner hunger. |
| Thursday | HIIT Workout (20 minutes) | At dinner, swap white pasta for a whole-grain or bean-based version. |
| Friday | Active Recovery (Yoga or Stretching) | Fill half your dinner plate with non-starchy vegetables. |
| Saturday | Long Walk or Hike | Enjoying a treat? Pair it with some protein or fat to soften the blood sugar spike. |
| Sunday | Rest or Gentle Movement | Plan your meals for the upcoming week to make staying on track feel effortless. |
This new playbook is about making strategic, sustainable changes that honor where your body is right now. For some women, these lifestyle shifts are enough. For many others, however, a more supported approach is needed to finally see real results.
If you feel like you're doing everything right but the scale won't budge, it might be time to look into personalized medical support. You can learn more about your options by taking the first step on your journey with Blue Haven Rx.
When to Consider Medical Support
For many women, there comes a point where even the most disciplined diet and exercise routine just isn't cutting it. If you feel like you're doing everything right but that stubborn perimenopause weight gain belly won't budge, please know you're not failing. It's simply a sign that your body's chemistry has changed, and it might need a different kind of support to get back on track.
Sometimes, you have to ask if what you've always done is still working for you now.
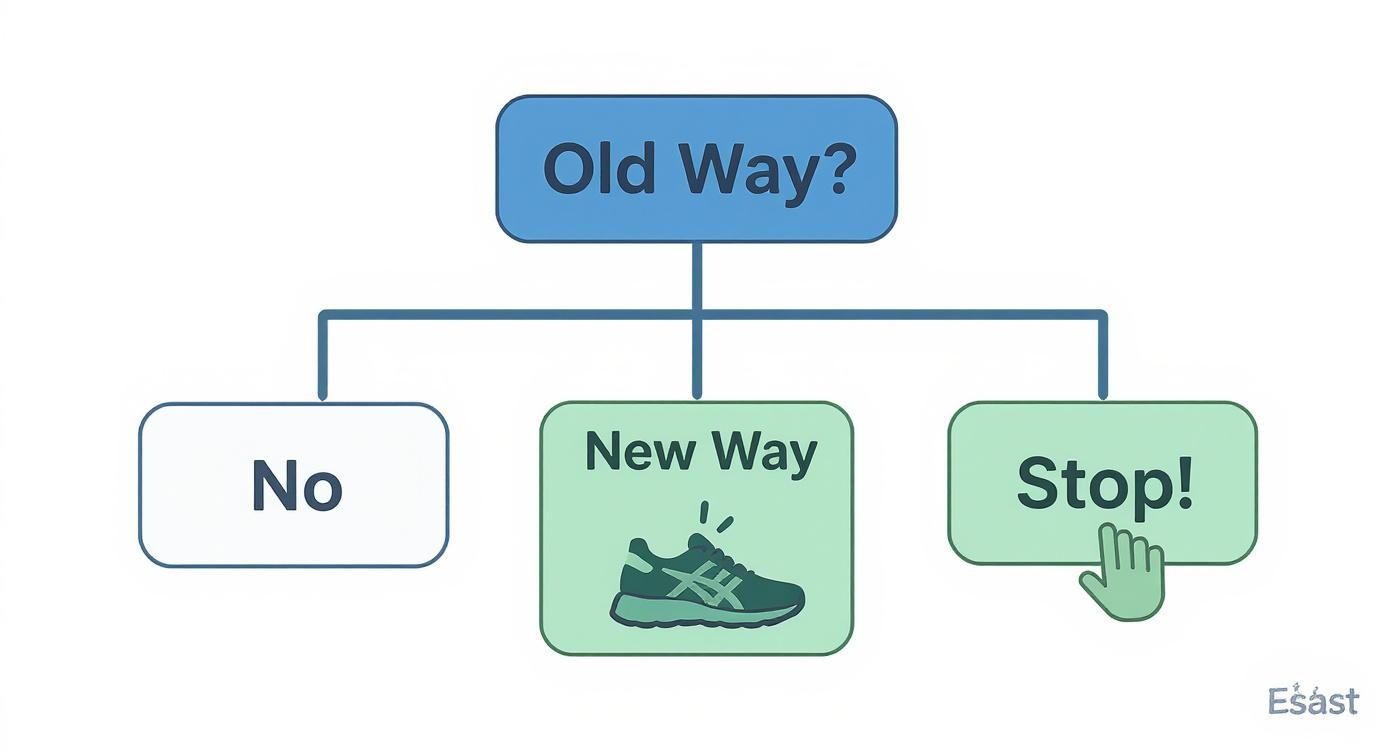
As this flowchart shows, continuing with old methods that no longer deliver results is a dead end. It might be time for a new strategy for your healthy living journey.
More Than Just Weight
Let's shift the conversation about perimenopausal weight gain away from the number on the scale and toward long-term health and longevity. That deep, visceral fat accumulating around your midsection isn't just a cosmetic frustration; it's a real health concern. This type of fat is metabolically active, churning out inflammatory substances linked to an increased risk of type 2 diabetes, heart disease, and high blood pressure.
Thinking about medical support isn't giving up—it’s the opposite. It’s a proactive, responsible choice to protect your future health. Exploring medical options is a testament to your commitment to your well-being. It means you’re ready to use every available tool to feel your best during this new chapter of life.
The Rise in Midlife Health Risks
The link between this life stage and health risks is clear in credible research. Perimenopause often triggers a sharp rise in abdominal obesity, which carries serious metabolic consequences. In the United States, for instance, obesity prevalence in women jumps from 39.7% in the 20-39 age group to 43.3% for those aged 40-59. It's not just about gaining fat; it's a specific shift toward more dangerous abdominal fat and less lean muscle, which directly raises the risk for chronic diseases. You can read the full research on perimenopausal metabolic changes to dig deeper into the science.
Personalized Medical Weight Management
Today’s medicine offers sophisticated, personalized programs that work with your body, not against it. These aren't one-size-fits-all diet plans. Instead, a well-designed medical plan is tailored to address the specific hormonal and metabolic hurdles you're facing during perimenopause.
A comprehensive program can give you access to:
- Expert Medical Guidance: Consultations with licensed physicians who understand the complexities of midlife weight gain.
- Advanced Tools: Prescription options that can help regulate appetite, improve how your body uses insulin, and break through frustrating weight loss plateaus.
- Ongoing Support: Continuous care from a team that can make adjustments as you progress, ensuring your plan remains effective.
This approach puts you back in the driver's seat. It’s about finding the right combination of lifestyle habits and medical support that creates real, lasting results. If you’re ready to see what a personalized plan could look like for you, the first step is to see if you’re a candidate. You can start your health journey today by taking our quick quiz.
How GLP-1 Medications Can Help
When you’ve tried everything—cleaned up your diet, committed to exercise—and the scale still won't budge, it’s easy to feel defeated. But sometimes, willpower alone isn't enough to fight back against biology. This is where modern medicine can offer a powerful assist.
For many women struggling with the stubborn perimenopause weight gain belly, prescription medications like GLP-1s are proving to be a true breakthrough. These aren’t magic pills. Think of them as scientific tools that help realign your body’s own systems, which have been thrown off by hormonal shifts.
GLP-1s essentially turn down the volume on the "food noise" that perimenopause can dial way up. They work by mimicking a hormone your gut naturally produces to signal fullness to your brain. The result? You feel satisfied with less food, which helps stop those overwhelming, hormone-fueled cravings that can feel impossible to ignore.
Addressing the Root Metabolic Issues
But GLP-1s do more than just manage appetite; they get to the heart of the metabolic problems that define this life stage. One of their biggest benefits is how they improve your body's response to insulin.
As we covered earlier, insulin resistance is a major culprit behind belly fat storage during perimenopause. By making your body more sensitive to insulin again, GLP-1s help break that vicious cycle of high blood sugar and fat accumulation right where it starts.
This one-two punch—quieting hunger while fixing metabolic function—is what makes these medications so effective for women in this phase of life. They don't replace your healthy habits; they make them work better. GLP-1s help bridge the gap between your efforts and your results. They are designed to work alongside healthy lifestyle changes, amplifying their effectiveness and helping you finally see the progress you deserve.
A Modern Approach to Care
Getting expert medical advice and access to these advanced treatments has never been easier. Telehealth services like Blue Haven Rx offer a private and convenient way to talk with licensed physicians who specialize in the unique challenges of midlife weight management.
This new way of getting care has some serious advantages:
- Personalized Plans: A doctor can review your health history and goals to see if a GLP-1 medication is a safe and appropriate option for you.
- Expert Guidance: You get continuous support from a medical team that monitors how you're doing and can fine-tune your plan along the way.
- Total Convenience: Consultations are done from home, on your schedule. If you're prescribed medication, it’s shipped discreetly to your door.
This kind of dedicated, personalized support can be the missing piece for achieving lasting results. To get a deeper dive into the science behind these medications, you can read our complete guide to GLP-1s for weight loss.
Ultimately, this is about using every available tool to feel strong, healthy, and in control. By pairing smart lifestyle choices with the right medical support, you can reclaim your health and feel like yourself again.
It’s Time to Write Your Next Chapter
Dealing with the changes perimenopause brings, especially that stubborn belly fat, can feel frustrating. But you absolutely have the power to manage it with the right game plan. This isn’t about chasing perfection; it's about making small, consistent steps that add up to big results for your long-term health and wellness.
You now understand the "why" behind it all—the hormonal rollercoaster of estrogen, cortisol, and insulin that’s re-writing the rules for your body. The old tricks just don't work anymore. Instead, your new playbook is built on a foundation of protein-rich nutrition, strength training, and giving stress and sleep the attention they deserve. These are non-negotiable for healthy living.
What's Your Next Step?
Knowing when to ask for help is a sign of strength. This journey is about so much more than what the scale says. It's about getting your energy back, safeguarding your health for the decades to come, and feeling confident in your own skin. This is your time to be proactive. Deciding to get a personalized plan isn't admitting defeat—it's a powerful declaration that you're investing in your long-term well-being.
Your body is playing by a new set of rules. It’s time you had a strategy that respects them. At Blue Haven Rx, we understand. We build personalized plans designed for your unique physiology during this specific phase of life. If you're ready to explore a supportive path forward and regain a sense of control, we're here to help.